I was in the stairwell close to the 5th floor of the nursing home where my grandmother resides when the phone rang. I paused, startled by the ring, and trying to suppress my slightly out of shape panting before I acknowledged the call clearly coming from the medical office we had visited earlier that day.
It was Tuesday the 11th. “Spring Break” had begun Saturday the 8th. Early that Saturday morning I had left on a road trip alone to the Marine Corps Base in Quantico where I had the privilege of watching a Marine who served with my Dad receive the Bronze Star with Valor – almost 50 years after the day it was earned. It was a whirlwind trip – 5 hours down that morning, and a busy, fun, emotional day that lasted well past midnight. I returned to Staten Island by 12:30 PM Sunday, in time to catch Meghan’s 1 PM Swim meet. Felix took “off” the workweek and spent Monday and Tuesday overseeing the installation of air conditioning in our house. It was 24 hours well spent – 12 each day- but the inevitable trail of dust and dirt needed to be tended to as well. So, I had headed to this appointment alone with Meghan earlier in the day. Now I was trying to visit with Grandma, although she’s often unsure I was ever there… I still know.

I took a deep breath before I answered.
A lovely young woman, whose cheery voice caused me to immediately forget her name asked, “Is this Meghan’s mother?” That is my favorite title- depending on whose asking. I tried my best to muster and equally cheery, “Yes, it is.”
“Oh, good. I was asked to set up Meghan’s surgical date.”
Sigh, Even though I knew the call was coming – it doesn’t get easier. I also knew I had very specific directions from Meghan that I was to “get it done as fast as possible.”
“How soon can we do this?” I asked.
“My first available is May 11th.”
“REALLY? A whole month?” I thought of the anticipation and the anxiety that would build as the pain increased. Then I realized something worse. May 11th is opening night for “Bye Bye Birdie,” her school play. Cast as Rosie she’s been preparing forever. There was just no way. I swallowed hard.
“What if I can’t take that date?” I held my breath,
Cheery changed her tune. I’m sure she thought I was being difficult. I tried to explain. No luck.
“The next date is May 20th, then you’re into June.”
I was playing out the June calendar in my brain. ComicCon with Dad, school dance, graduation, West Virginia… forget about the Long Course Swim Season and the 2 meets we knew she’d have to scratch out of, and the last CYO Swim meet she’d ever be eligible for- that was out too.
There was never going to be a good time to be out of commission.
Deep breath. “Any chance you’ll have cancellations?”
“No.”
“Ok then. May 20th it is.”
And after telling me I’d need to give up a day the week before for formal pre-surgical testing, which is a first for us, as she grows up, I didn’t bother to explain I’d just missed 16 days of work for vocal cord surgery. I just said, “Thank you.”
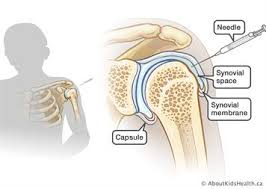
Meghan’s relationship with her right knee is complicated. It started giving her trouble before she could talk, as her first babysitter will attest to hours rubbing that knee. As she grew, it got worse. It always seemed to bother her. She pushed, and pushed. Eventually it was hot to the touch and pulsating. The diagnosis came in 2008, after multiple mis-diagnoses, including “her pants are too tight.” Finally, a team at Sloan Kettering, adept at ruling out cancer, was able to diagnose a high flow arteriovenous malformation (AVM) in that knee. We were sent off to Interventional Radiology at Lenox Hill, where the doctor confidently told us he could eliminate this AVM in “one procedure – 2 tops.” Between December of 2009 and February of 2012 there were 4 embolizations on that knee.

The doctor seemed almost relieved when she was diagnosed with Cowden’s Syndrome in the fall of 2011. It seemed as if he felt better about himself, like there was another explanation to justify why the darn thing just wouldn’t quit. By that point she was being run through the surgical mill, so we welcomed the 2 and a half years of monitoring. It seemed to stabilize.
But, as everything overlaps and one thing leads to another, there was pain. There was pain that she was repeatedly told should not be there. Yet, no matter what they said, the pain was there, and it was consistent, and it was real. She pressed through. She stopped soccer and tried dance. The knee was cut out for neither. She found her way into the pool in the spring of 2013.
By that fall we had signed her up for a 12 month competitive swim team, and things were looking up. She swam a full year, getting stronger, becoming more confident, and finally feeling like an athlete.

There were other surgeries in between. And there was that knee pain.She had been prescribed Celebrex to substitute for the Advil that was being consumed in clearly excessive quantity to allow her to function. And the Celebrex was wonderful. Until it wasn’t.
And in May of 2014, two months after a complete thyroidectomy (thank you Cowden’s) she lay in the hospital in severe GI distress. It took a week to stabilize her. I was scared. Out went the Celebrex, fried food, and a whole host of other goodies.
But, little did I realize, that Celebrex was likely the reason the AVM had quieted down. Apparently the drug has properties that work on blood flow. A few months off of the Celebrex and all hell broke loose. Literally. It was November of 2014, the Tuesday night before Thanksgiving when she collapsed outside of swim practice, unable to walk. Our travels that night took us directly to Lenox Hill ER because we were sure it was the AVM in action again.
Proven right when the surgeon showed up early the next morning giving me a surgical time for her, they drained 50ccs of blood from the knee that day.

Blood and bone and tissue are not friendly. It’s like neighbors invading space. You can tolerate it for a while, but it doesn’t take long before the damage is irreparable. It became evident there was structural damage beginning because the blood had begun to wear things away and allow the knee cap to move to places it did not belong.
We were advised to consult with an orthopedist, and we did. He wanted a coordinated arthroscopy where both he and the interventional radiologist would be in the OR together. It became an orthopedic procedure. The patella was moved back where it belonged. Things were cleaned out. Recovery was smooth relative to the emobolizations. We were told it would last a few years.
In January 2017 we were pretty much released from interventional radiology. We were told the AVM seemed quiet and we need only bring her back if she becomes symptomatic again. In February the knee pain started again. Slow, but steady, it kept growing in duration and consistency. At a routine visit the orthopedist mentioned the potential need for another arthroscopy. He reviewed the January MRI and showed us where the patella had shifted again. He said her growth plates were “wide open” (a scary thought at over 5’7″) and that this would continue to be an issue at least until she finishes growing. He offered her a “patella stabilizing brace” for 6 weeks, to see if it would do the job he wanted done.
Tuesday the 11th he looked at her knee for less than 2 minutes before he started making plans for the surgery. He explained to us what he needed to cut and move, and why it was time to get it done. We had the necessary conversations about length of time out of the pool, and other restrictions. We left, quiet and resolved. The only thing she asked me was to just get it done as soon as possible.

So when the phone rang in the hall last Tuesday afternoon, I felt sucker-punched, again. Regardless of how many times I tell myself, and her, that it “could be worse” and we have to “look at the bright side,” the reality is that sometimes it sucks. And that’s just the frank honest truth. Scheduling your 7th knee surgery in 13.5 years is just not ok, not even a bit. I was grateful for Grandma, and the ability to be distracted for a bit. Without her memory, she is just real. That was a good day. And that day she loved having me. I cherished the visit.
I spent Wednesday in the grocery shopping marathon, and Wednesday night at swim.
Thursday was for an extensive blood draw for Meghan and a triple dermatologist appointment. Meghan headed to play practice, and I traveled to my vocal follow up in NYC.
My report was adequate, but not what I had hoped for. Still swelling. Still be very careful. Still rest when you can. Still exercise caution when you get back into your program on the 19th.
Friday was for vocal therapy. And for trying to put the house back together. And for painting upstairs, and washing the dist off the curtains, and visiting my in-laws. It was our 17th Anniversary. We sneaked an hour or two for dinner together…
Saturday was voice lessons, and…
Somehow it bled into Sunday, and Easter and some time with family. But, it was immediately back to the painting.
By Monday I was waiting for the blood results, hoping to catch a call from one of the three doctors on the order. We hit the orthodontist to have the retainer tightened, and a few things at Costco before it was time for swim…
I am focusing on the sunny days. I am trying to find some time within the chaos to be still.
I asked Meghan why she was so uptight the other day. It really was a stupid question. This was the grossly abbreviated version of ONE aspect of her real life.

And tomorrow she will have to practice smiling and responding to the question “How was your break?” in the only socially acceptable way. “It was fine, how about you?”
Fine… it has so many meanings. We don’t want to bring people down all the time. It gets hard to have a conversation sometimes though. Felix and I realized in the years since we’re married, one of us has been in an operating room somewhere in the neighborhood of 34 times. A lot of our days are spent recovering. Physically, mentally and emotionally recovering. Fighting financially against incorrect billing, and generally trying to breathe.
I’ve said it before and I’ll say it again, we would not trade our lives for anyone’s. However, just like in anyone’s life, some days are better than others.
I’m anxious for a vacation not peppered with appointments and surgeries.
Until then, maybe I should teach Meghan to answer “How was your vacation?” with “It’s complicated…”
#beatingcowdens